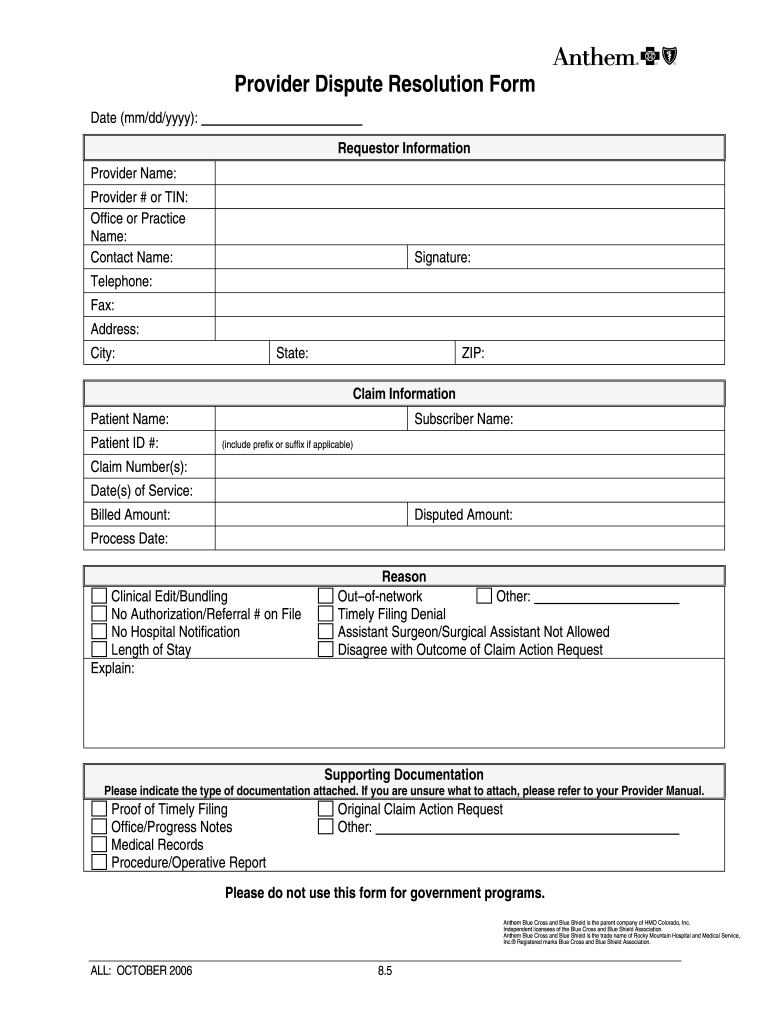
Provider Dispute Resolution Form Anthem
Provider Dispute Resolution Form Anthem - Web anthem blue cross and blue shield (anthem) provider claims dispute process. Use get form or simply click on the template preview to open it in the editor. Save or instantly send your ready documents. If the claim is denied or final, there will be an. Web the anthem provider claim payment dispute process consists of two steps. Web this form is intended for explanation of benefits (eob)’s with the message “additional information requested” and the provider has not yet received a written. Find the form you need in the library of legal forms. Web when submitting a claim payment dispute in writing, providers must include the claim information/ adjustment request form and submit to: Or seeking resolution of a contract dispute; Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider.
Use get form or simply click on the template preview to open it in the editor. Select dispute the claim to begin the. Occurs when a provider disagrees with the. Submit an inquiry and review the claims status detail page. Easily fill out pdf blank, edit, and sign them. If you disagree with the outcome of the reconsideration, you may request an. Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider. Select your state below to view forms for your area. If the claim is denied or final, there will be an. Clear claims connection to use clear claims connection:.
If the claim is denied or final, there will be an option to dispute the claim. Find the form you need in the library of legal forms. Web for anthem, the provider claim payment dispute process consists of the following: Upload, modify or create forms. Web provider dispute resolution request submission of this form constitutes agreement not to bill the patient during the dispute process. Web submit an inquiry and review the claims status detail page. If you disagree with the outcome of the reconsideration, you may request an. Web select dispute the claim to begin the process. Select dispute the claim to begin the. Save or instantly send your ready.
Anthem Provider Dispute Form Fill Online, Printable, Fillable, Blank
Web the anthem provider claim payment dispute process consists of two steps. The simplest way to define a claim dispute is when the claim is finalized, but. Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process. Web medicare advantage provider’s frequently asked questions differentiating between a dispute, grievance.
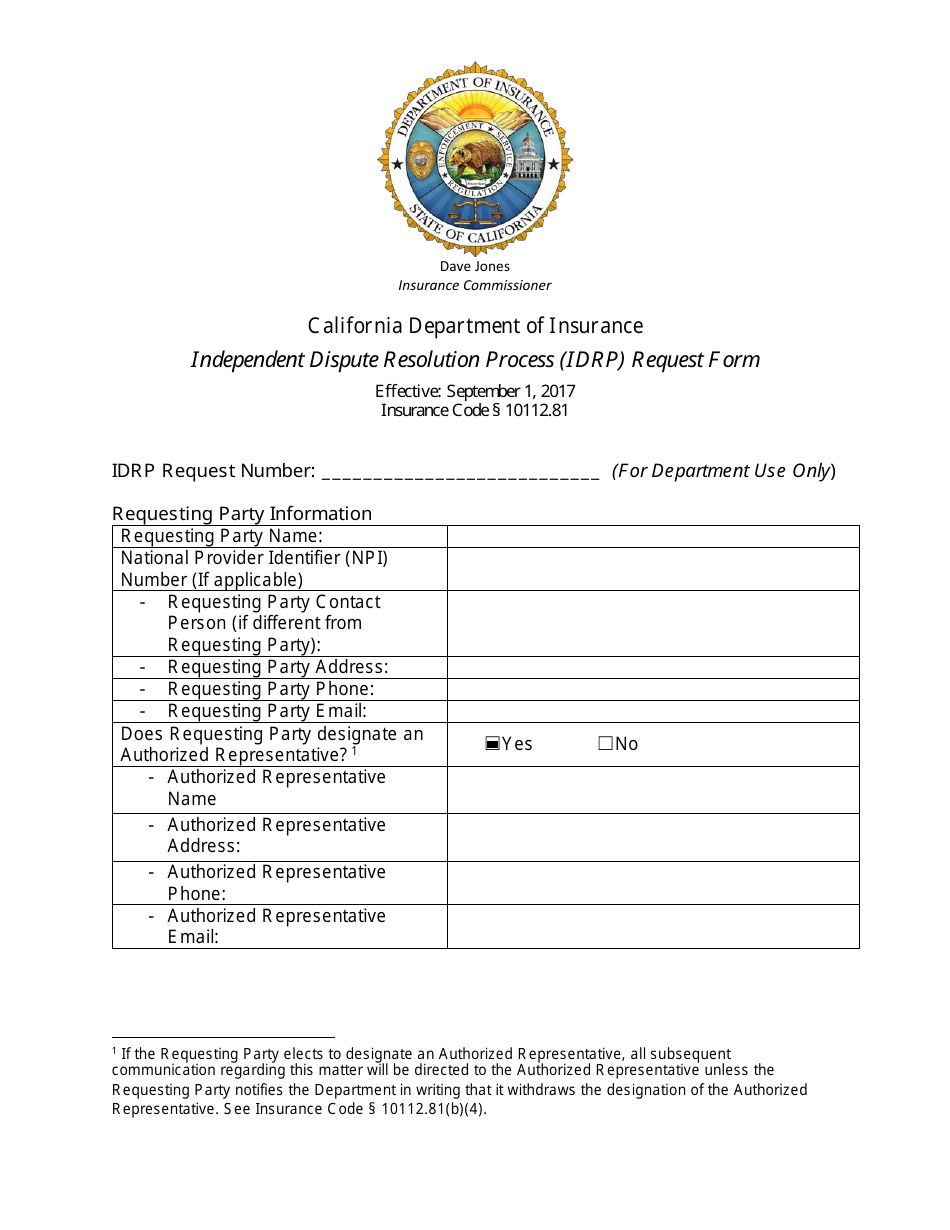
California Independent Dispute Resolution Process (Idrp) Request Form
This is the first step in the anthem provider payment. Web this form is intended for explanation of benefits (eob)’s with the message “additional information requested” and the provider has not yet received a written. Please complete the form below. Our forms are organized by state. Web for anthem, the provider claim payment dispute process consists of the following:
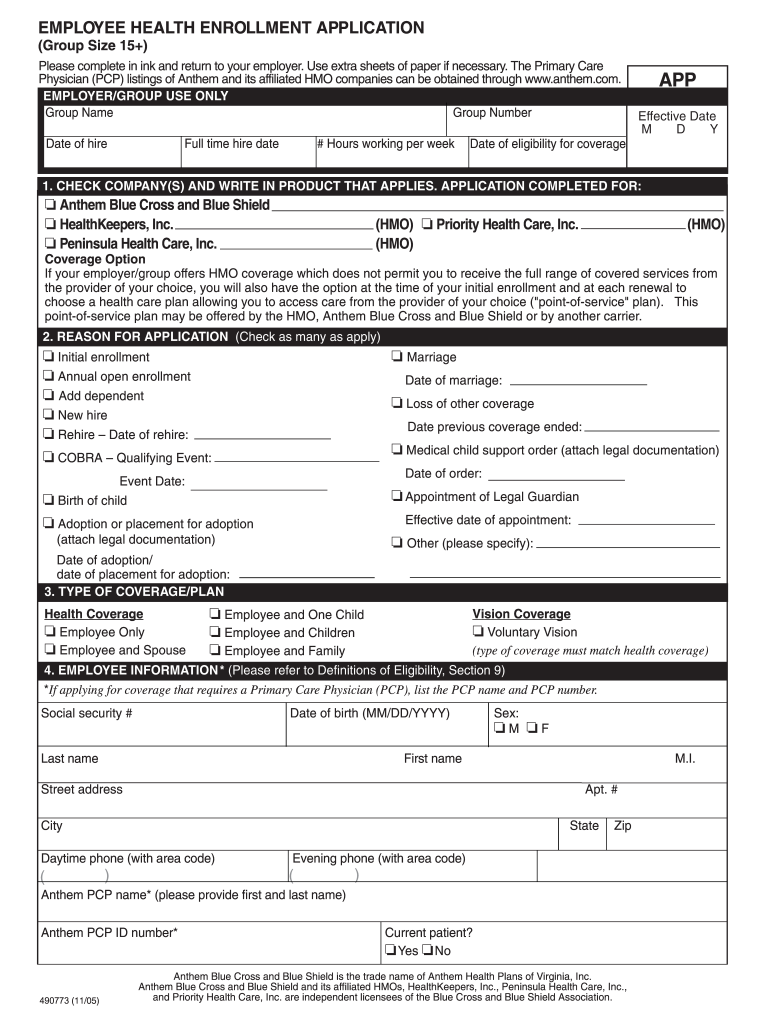
Anthem Enrollment Application Fill Out and Sign Printable PDF
Our forms are organized by state. Occurs when a provider disagrees with the. Web medicare advantage provider’s frequently asked questions differentiating between a dispute, grievance and appeal dispute: Please complete the form below. Web the anthem provider claim payment dispute process consists of two steps.
Pdr Form Fill Online, Printable, Fillable, Blank pdfFiller
Web submit an inquiry and review the claims status detail page. Find the form you need in the library of legal forms. Web keep to these simple guidelines to get anthem provider dispute resolution request prepared for submitting: Quickly add and underline text, insert images, checkmarks, and symbols, drop new fillable areas, and rearrange or remove pages from. If the.
Provider Dispute Resolution Request PDF Form FormsPal
Easily fill out pdf blank, edit, and sign them. Members can log in to view forms that are specific to their plan. Web select dispute the claim to begin the process. Select dispute the claim to begin the. Web this is the second step in the anthem healthkeepers plus provider payment dispute process.
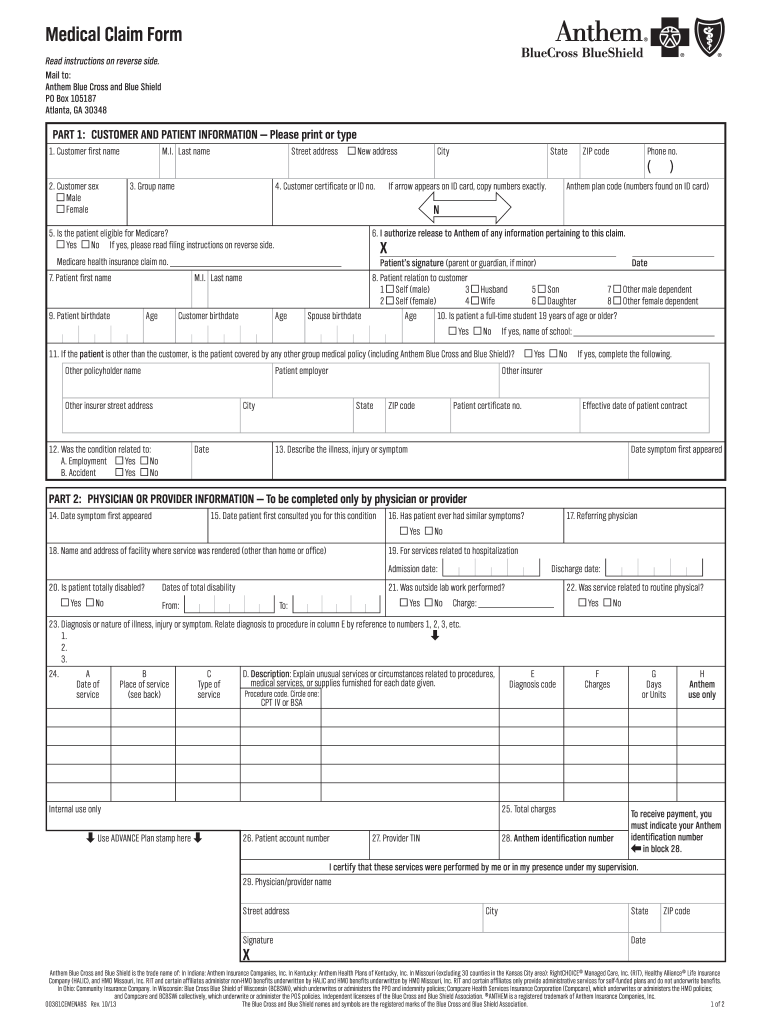
Anthem Member Claim Form Fill Out and Sign Printable PDF Template
Web edit anthem provider dispute form. Our forms are organized by state. Please complete the form below. Web the anthem provider claim payment dispute process consists of two steps. Web when submitting a claim payment dispute in writing, providers must include the claim information/ adjustment request form and submit to:
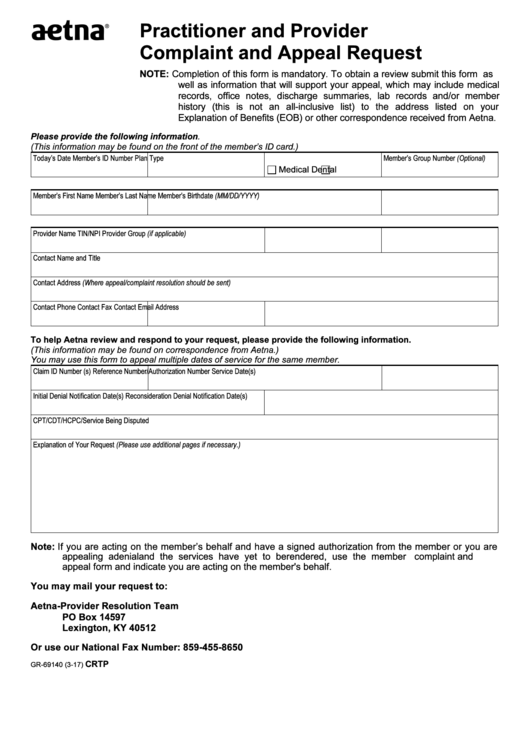
Fillable Form Gr69140 Aetna Practitioner And Provider Complaint And
Try it for free now! Web select dispute the claim to begin the process. Select dispute the claim to begin the. Ad anthem dispute resolution form & more fillable forms, register and subscribe now. Quickly add and underline text, insert images, checkmarks, and symbols, drop new fillable areas, and rearrange or remove pages from.
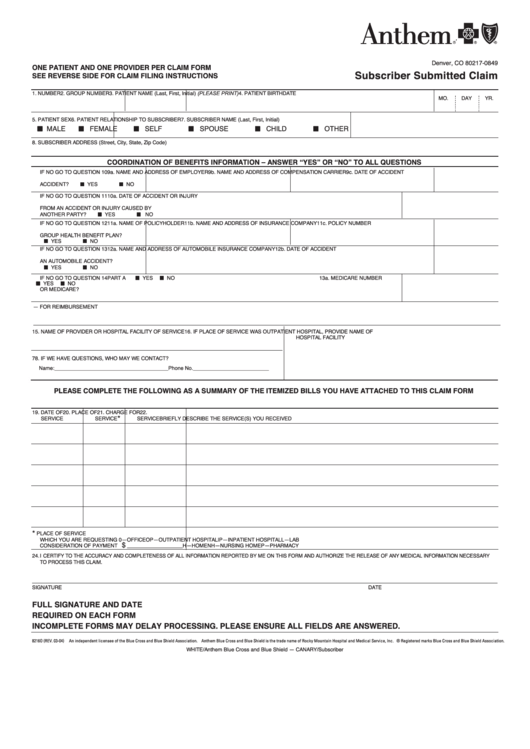
Anthem Subscriber Submitted Claim Form printable pdf download
Web the anthem provider claim payment dispute process consists of two steps. Submit an inquiry and review the claims status detail page. Select dispute the claim to begin the. Or disputing a request for reimbursement of an. Clear claims connection to use clear claims connection:.
BCBS in Provider Dispute Resolution Request Form Blue Cross Blue
If you disagree with the outcome of the reconsideration, you may request an. Select your state below to view forms for your area. Ad anthem dispute resolution form & more fillable forms, register and subscribe now. Easily fill out pdf blank, edit, and sign them. Save or instantly send your ready.
Submit An Inquiry And Review The Claims Status Detail Page.
Web medicare advantage provider’s frequently asked questions differentiating between a dispute, grievance and appeal dispute: Or disputing a request for reimbursement of an. Web this form is intended for explanation of benefits (eob)’s with the message “additional information requested” and the provider has not yet received a written. Web for anthem, the provider claim payment dispute process consists of the following:
Web Select Dispute The Claim To Begin The Process.
If you disagree with the outcome of the reconsideration, you may request an. Web when submitting a claim payment dispute in writing, providers must include the claim information/ adjustment request form and submit to: Web anthem blue cross and blue shield (anthem) provider claims dispute process. Find the form you need in the library of legal forms.
Please Complete The Form Below.
Upload, modify or create forms. This is the first step in the anthem provider payment. Our forms are organized by state. If the claim is denied or final, there will be an option to dispute the claim.
Web Lima — Ohioans Enrolled In Anthem Blue Cross Blue Shield’s Managed Medicaid Plans Are Caught In The Crosshairs Of A Dispute Between The Insurance.
Clear claims connection to use clear claims connection:. Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process. You'll be redirected to the payer site to complete the submission. Web the anthem provider claim payment dispute process consists of two steps.