Highmark Blue Cross Blue Shield Prior Authorization Form
Highmark Blue Cross Blue Shield Prior Authorization Form - Brunory, janet (doi) created date: A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. Web updated june 02, 2022. All inpatient admissions, including organ transplants. Select the appropriate highmark blue shield form to get started. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional information as specified: Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts. Designation of authorized representative form. Some authorization requirements vary by member contract. Inpatient and outpatient authorization request form.
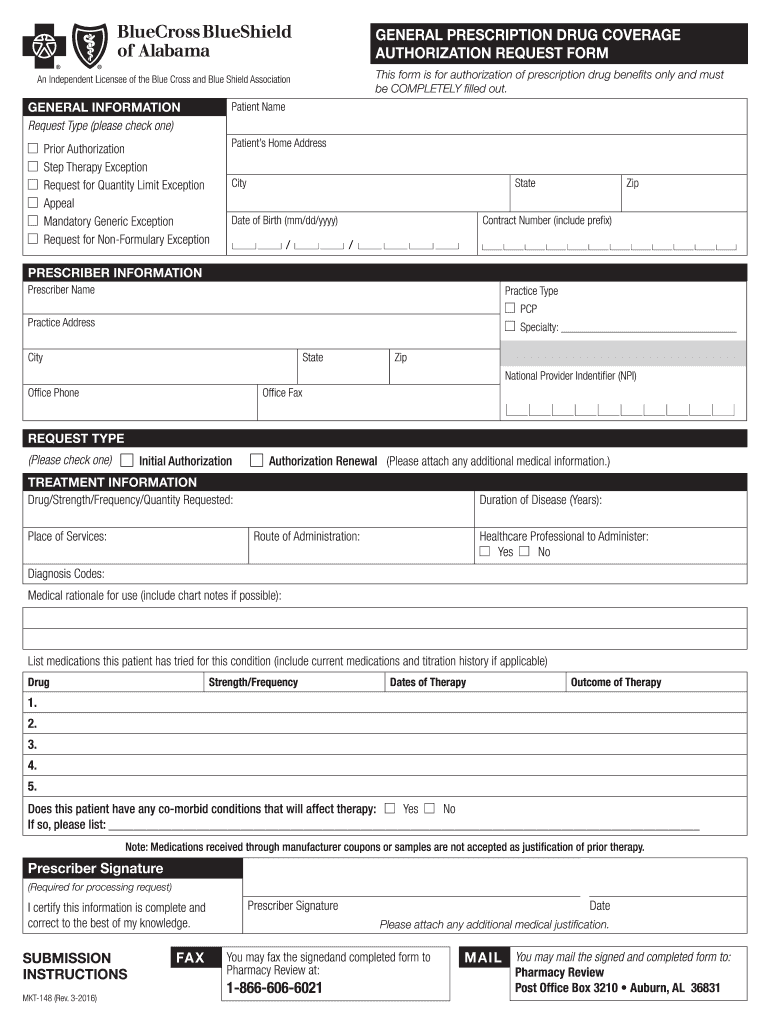
Highmark blue cross blue shield, highmark choice company, highmark health insurance company, highmark coverage advantage, highmark benefits group, highmark senior health company, first priority health and/or first priority life provide health benefits and/or health benefit administration in the 29. The authorization is typically obtained by the ordering provider. Designation of authorized representative form. Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts. A physician must fill in the form with the patient’s member information as well as all medical details related to the requested prescription. Web prior authorizations are required for: Web updated june 02, 2022. Select the appropriate highmark blue shield form to get started. Some authorization requirements vary by member contract.
Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional information as specified: Some authorization requirements vary by member contract. Web updated june 02, 2022. Web prior authorizations are required for: Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service. All inpatient admissions, including organ transplants. Any service that requires an authorization from a primary payer, except nonexhausted original medicare services. Highmark blue cross blue shield, highmark choice company, highmark health insurance company, highmark coverage advantage, highmark benefits group, highmark senior health company, first priority health and/or first priority life provide health benefits and/or health benefit administration in the 29. Web highmark blue shield has partnered with covermymeds to offer electronic prior authorization (epa) services. Web 76168de0720001 my blue access major events ppo catastrophic 9450 + 3 free pcp visits 21 $ 274.65 $ 281.52 76168de0730001 my blue access ppo premier gold 0 21 $ 471.19 $ 482.97.
Blue cross blue shield pennsylvania highmark availity
Durable medical equipment over $500. Designation of authorized representative form. A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. Web updated june 02, 2022. Web 76168de0720001 my blue access major events ppo catastrophic 9450 + 3 free pcp visits 21 $ 274.65 $ 281.52.
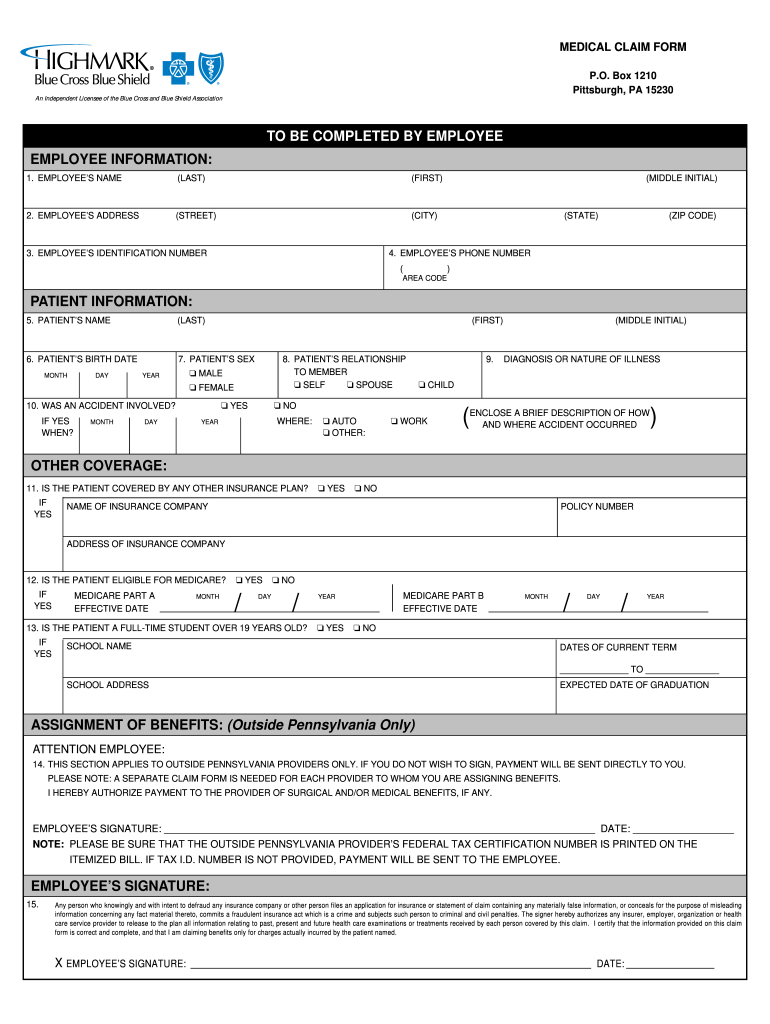
Highmark blue cross blue shield submit claim
Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service. Web updated june 02, 2022. Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Brunory, janet (doi) created date: Designation of authorized representative form.
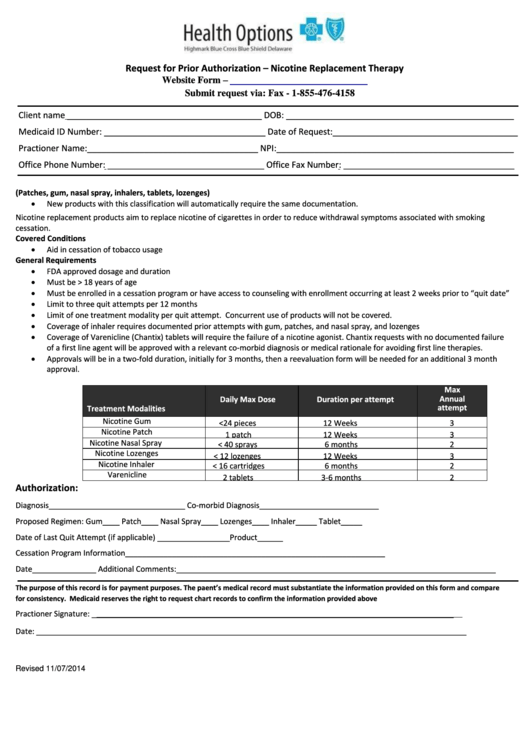
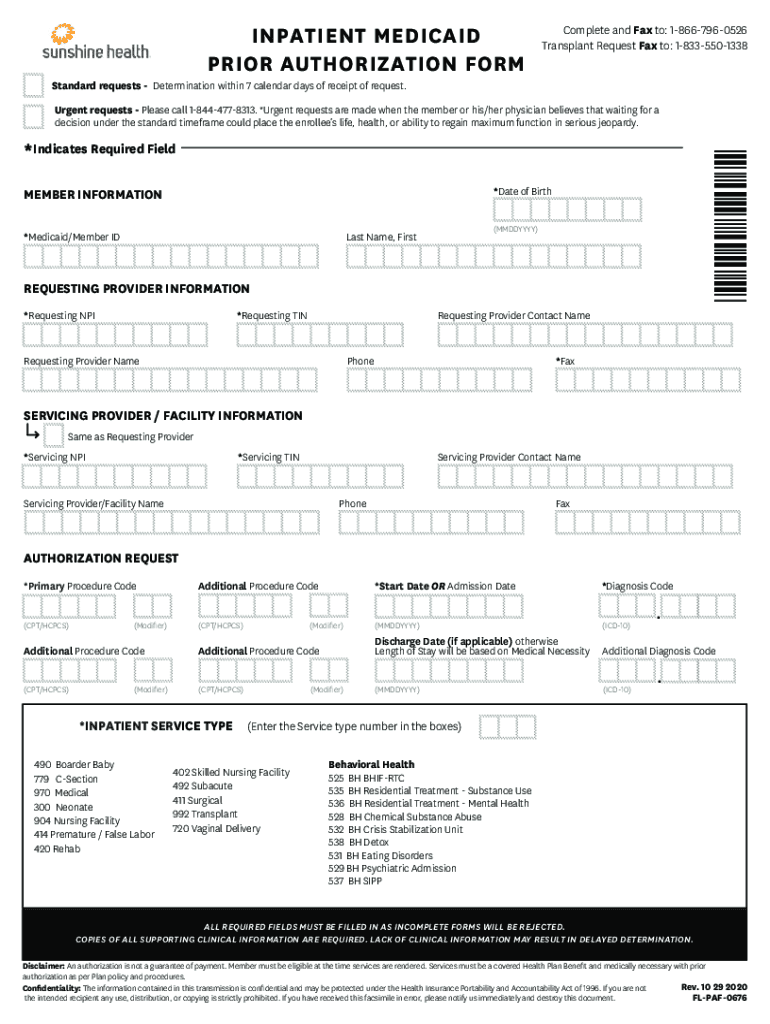
Request For Prior Authorization Form Highmark Blue Cross Blue Shield
Brunory, janet (doi) created date: Inpatient and outpatient authorization request form. Durable medical equipment over $500. Designation of authorized representative form. A physician must fill in the form with the patient’s member information as well as all medical details related to the requested prescription.
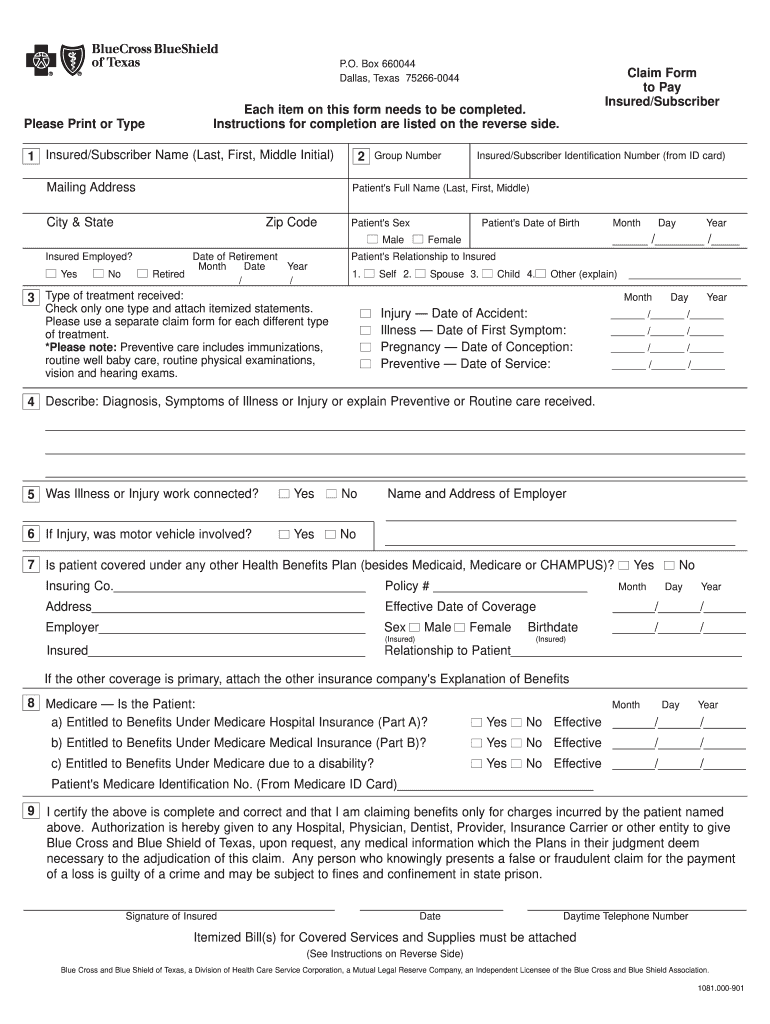
Bcbs Claim Form Fill Out and Sign Printable PDF Template signNow
Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service. Web updated june 02, 2022. All inpatient admissions, including organ transplants. Highmark blue cross blue shield, highmark choice company, highmark health insurance company, highmark coverage advantage, highmark benefits group, highmark senior health company, first priority.
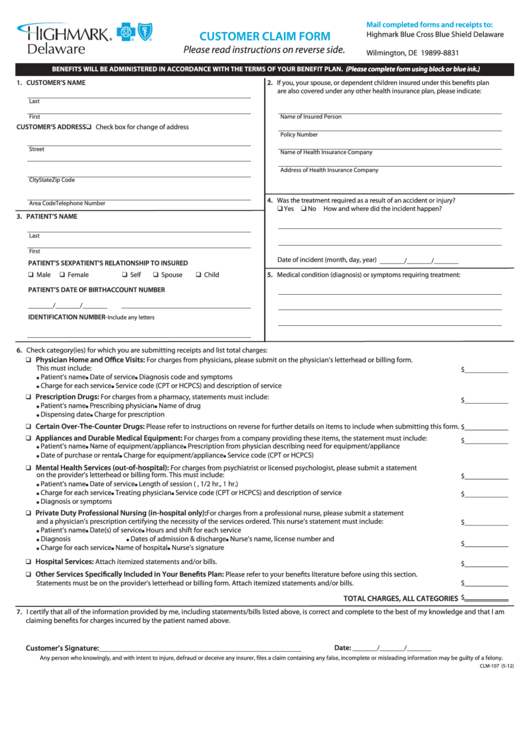
Customer Claim Form Highmark Blue Cross Blue Shield Delaware
Inpatient and outpatient authorization request form. Brunory, janet (doi) created date: Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service. Web prior authorizations are required for: A physician must fill in the form with the patient’s member information as well as all medical details.
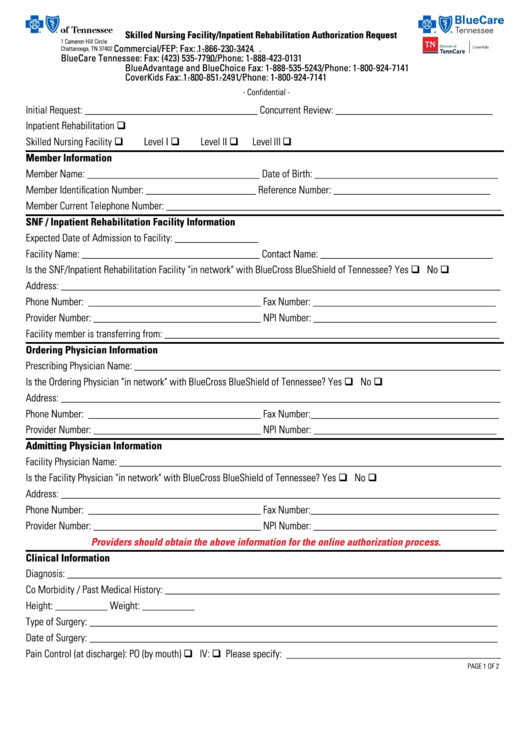
Priority Health Inpatient Authorization Form Fill Out and Sign
Inpatient and outpatient authorization request form. Web updated june 02, 2022. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional information as specified: A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health.
ASC Coding and Billing Fundamentals Objectives PDF
Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service. Inpatient and outpatient authorization request form. Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Any service that requires an authorization from a primary payer, except nonexhausted original medicare services..
2008 Form AL BCBS MKT148 Fill Online, Printable, Fillable, Blank
Web prior authorizations are required for: Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Web updated june 02, 2022. Web 76168de0720001 my blue access major events ppo catastrophic 9450 + 3 free pcp visits 21 $ 274.65 $ 281.52 76168de0730001 my blue access ppo premier gold 0 21 $ 471.19 $ 482.97. Some authorization.
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates free
Web prior authorizations are required for: Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts. Highmark blue cross blue shield delaware. Inpatient and outpatient authorization request form. Any service.
Fill Free fillable Blue Cross and Blue Shield of Texas PDF forms
Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts. Durable medical equipment over $500. Inpatient and outpatient authorization request form. Web prior authorization for the following drugs and/or therapeutic.
A Physician Must Fill In The Form With The Patient’s Member Information As Well As All Medical Details Related To The Requested Prescription.
All inpatient admissions, including organ transplants. A highmark prior authorization form is a document used to determine whether a patient’s prescription cost will be covered by their highmark health insurance plan. Covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Web for providers provider manual and resources forms and reference material forms and reference material forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization request form attendant care monthly missed visits/hours/shifts.
Durable Medical Equipment Over $500.
Select the appropriate highmark blue shield form to get started. Web 76168de0720001 my blue access major events ppo catastrophic 9450 + 3 free pcp visits 21 $ 274.65 $ 281.52 76168de0730001 my blue access ppo premier gold 0 21 $ 471.19 $ 482.97. The authorization is typically obtained by the ordering provider. Web highmark requires authorization of certain services, procedures, and/or durable medical equipment, prosthetics, orthotics, & supplies ( dmepos) prior to performing the procedure or service.
Web Highmark Blue Shield Has Partnered With Covermymeds To Offer Electronic Prior Authorization (Epa) Services.
Inpatient and outpatient authorization request form. Any service that requires an authorization from a primary payer, except nonexhausted original medicare services. Web updated june 02, 2022. Highmark blue cross blue shield, highmark choice company, highmark health insurance company, highmark coverage advantage, highmark benefits group, highmark senior health company, first priority health and/or first priority life provide health benefits and/or health benefit administration in the 29.
Brunory, Janet (Doi) Created Date:
Designation of authorized representative form. Web prior authorizations are required for: Some authorization requirements vary by member contract. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional information as specified: