Fepblue Prior Authorization Form
Fepblue Prior Authorization Form - Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Fep offers three nationwide options for federal employees and retirees (standard option, basic option. Web february 2019 addition of statement: Web 1 results found for search term : Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. Web fep® blue focus www.fepblue.org 2023. Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. Web prior approval may be required for certain prescription drugs before they can be covered under the pharmacy benefit. Web the preferred provider network for fep is preferred patient care. Web fep prior approval program according to the terms of your coverage, prior approval is required for certain services and supplies and must be renewed periodically.
Massachusetts standard form for medication prior authorization requests (eform) or contact clinical. Web 2022 fep blue focus; Web fep® blue focus www.fepblue.org 2023. Coronavirus update fep will waive early. Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. Service benefit plan prior approval p.o. Web standard and basic option prior approval list fep blue focus prior approval list. Web to request prior authorization for these medications, please submit the: Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. However, some select drugs require your doctor to provide information about your prescription to determine coverage.
Fep offers three nationwide options for federal employees and retirees (standard option, basic option. Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Be the first to know about our benefits, wellness incentives and rewards you're eligible for with your plan. Web prior approval may be required for certain prescription drugs before they can be covered under the pharmacy benefit. Explore prior approval topics learn about prior. Web fep prior approval program according to the terms of your coverage, prior approval is required for certain services and supplies and must be renewed periodically. Brain cancer is not considered a form of head or neck cancer;. Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. Web get the latest from fep. Web to request prior authorization for these medications, please submit the:
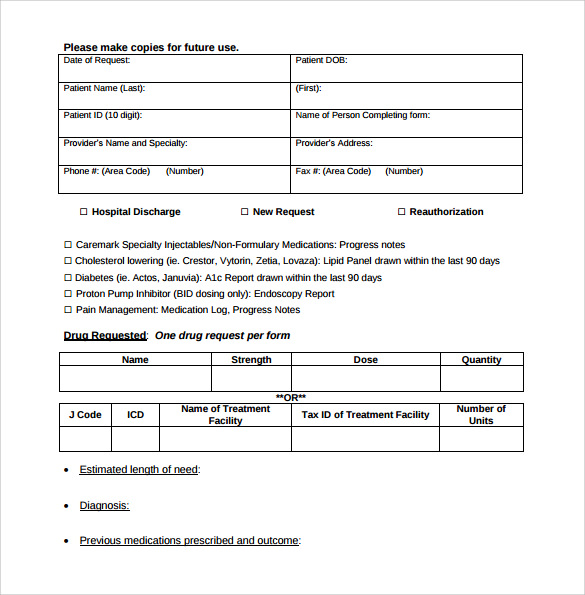
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Web 2022 fep blue focus; Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. Web the preferred provider network for fep is preferred.
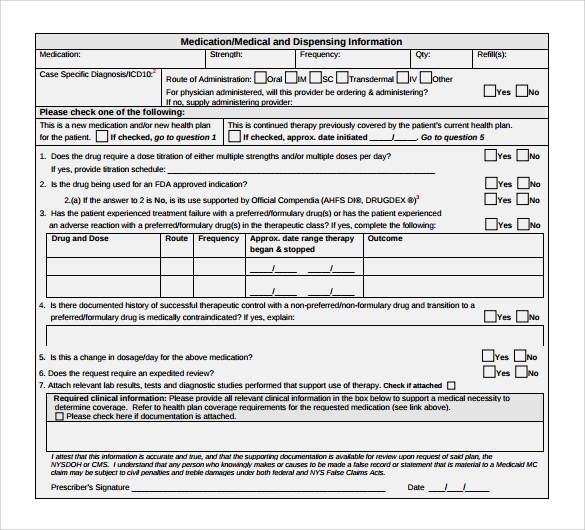
Covermymeds Prior Authorization Form Pdf Form Resume Examples
Web prior approval may be required for certain prescription drugs before they can be covered under the pharmacy benefit. Web the preferred provider network for fep is preferred patient care. Service benefit plan prior approval p.o. Fep offers three nationwide options for federal employees and retirees (standard option, basic option. Be the first to know about our benefits, wellness incentives.
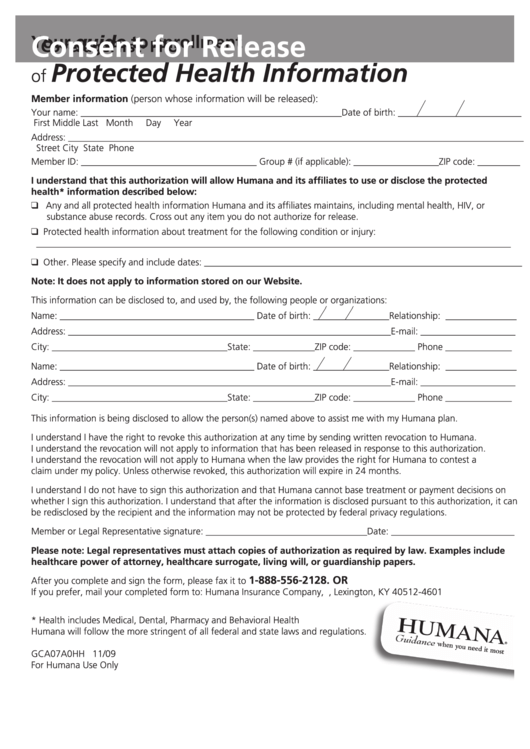
Fillable Consent For Release Of Protected Health Information printable
Service benefit plan prior approval p.o. Web 1 results found for search term : Effective on january 1, 2022 updated: However, some select drugs require your doctor to provide information about your prescription to determine coverage. Service benefit plan prior approval p.o.
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Web get the latest from fep. Web most drugs are covered without requiring prior approval. Explore prior approval topics learn about prior. Service benefit plan prior approval p.o. Web standard and basic option prior approval list fep blue focus prior approval list.
Fep Prior Authorization Form â
Coronavirus update fep will waive early. Web to request prior authorization for these medications, please submit the: December 23, 2021 prior approval is required for all imrt services except imrt related to the treatment of the. However, some select drugs require your doctor to provide information about your prescription to determine coverage. Massachusetts standard form for medication prior authorization requests.
Fep Blue Fill Online, Printable, Fillable, Blank pdfFiller
Web fep prior approval program according to the terms of your coverage, prior approval is required for certain services and supplies and must be renewed periodically. Brain cancer is not considered a form of head or neck cancer;. Web prior approval may be required for certain prescription drugs before they can be covered under the pharmacy benefit. Web february 2019.
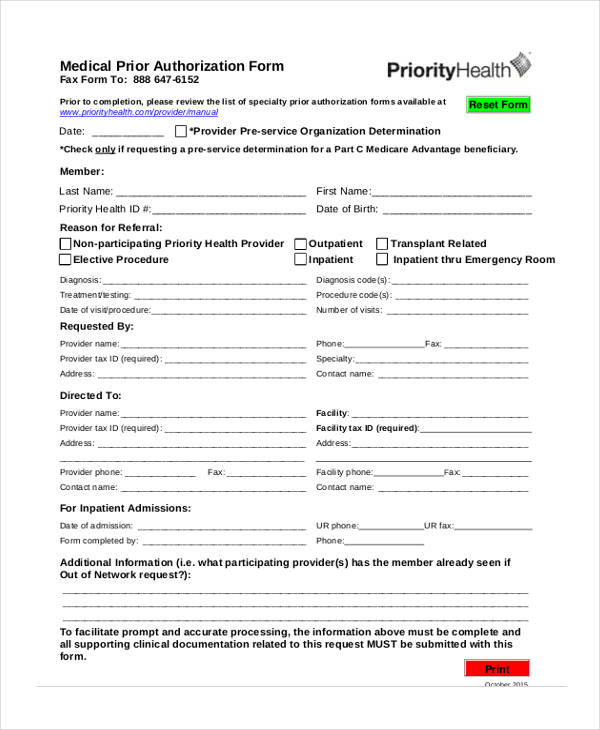
FREE 13+ Prior Authorization Forms in PDF MS Word
Web the preferred provider network for fep is preferred patient care. Massachusetts standard form for medication prior authorization requests (eform) or contact clinical. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Effective on january 1, 2022 updated: Web a prior approval, or pa, review determines medical necessity and considers fep benefits.
Medicare Generation Rx Prior Authorization Form Form Resume
Service benefit plan prior approval p.o. December 23, 2021 prior approval is required for all imrt services except imrt related to the treatment of the. Fep offers three nationwide options for federal employees and retirees (standard option, basic option. Be the first to know about our benefits, wellness incentives and rewards you're eligible for with your plan. Web 1 results.
Medicare Generation Rx Prior Authorization Form Form Resume
Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. Web a prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure, service, or supply is provided. Effective on january 1, 2022 updated: Brain cancer is not considered a form of head.
Bcbs Prior Authorization Form Tennessee Form Resume Examples
Service benefit plan prior approval p.o. Web to request prior authorization for these medications, please submit the: Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet.
However, Some Select Drugs Require Your Doctor To Provide Information About Your Prescription To Determine Coverage.
December 23, 2021 prior approval is required for all imrt services except imrt related to the treatment of the. Service benefit plan prior approval p.o. Be the first to know about our benefits, wellness incentives and rewards you're eligible for with your plan. Web prior approval may be required for certain prescription drugs before they can be covered under the pharmacy benefit.
Coronavirus Update Fep Will Waive Early.
Web 2022 fep blue focus; Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. Massachusetts standard form for medication prior authorization requests (eform) or contact clinical. Web february 2019 addition of statement:
Service Benefit Plan Prior Approval P.o.
Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Fep offers three nationwide options for federal employees and retirees (standard option, basic option. Web fep® blue focus www.fepblue.org 2023. Web to request prior authorization for these medications, please submit the:
Web Fep Prior Approval Program According To The Terms Of Your Coverage, Prior Approval Is Required For Certain Services And Supplies And Must Be Renewed Periodically.
Service benefit plan prior approval p.o. Web standard and basic option prior approval list fep blue focus prior approval list. Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. Web a prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure, service, or supply is provided.