Ambetter Provider Appeal Form
Ambetter Provider Appeal Form - Web prior to submitting a claim dispute, the provider must first submit a “request for reconsideration”. Claim reconsideration claim appeal authorization appeal provider name. You must file an appeal within 180 days of the date on the denial letter. Claim complaints must follow the dispute process and then the complaint process below. The claim dispute must be submitted within. Web ambetter provider reconsiderations, disputes and complaints (cc.um.05.01) to see if the case qualifies for medical necessity review. Web provider reconsideration and appeal request form use this form to request one of the following: See coverage in your area; The procedures for filing a. Web to ensure that ambetter member's rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process.
Web ambetter provides the tools and support you need to deliver the best quality of care. The procedures for filing a. Web provider request for reconsideration and claim dispute form use this form as part of the ambetter from sunshine health request for reconsideration and. Log in to the nch provider web portal at. Web prior to submitting a claim dispute, the provider must first submit a “request for reconsideration”. You must file an appeal within 180 days of the date on the denial letter. Web outpatient prior authorization fax form (pdf) outpatient treatment request form (pdf) provider fax back form (pdf) applied behavioral analysis authorization form (pdf). Web provider reconsideration and appeal request form use this form to request one of the following: Learn more about our health insurance. This could be a denial of coverage for requested medical care or for a claim you filed for.
The claim dispute must be submitted within. Web to ensure that ambetter member's rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. Web outpatient prior authorization fax form (pdf) outpatient treatment request form (pdf) provider fax back form (pdf) applied behavioral analysis authorization form (pdf). Web appeal you file an appeal in response to a denial received from ambetter from health net. See coverage in your area; Web appeal by phone, fax, or in person. Web ambetter provider reconsiderations, disputes and complaints (cc.um.05.01) to see if the case qualifies for medical necessity review. An appeal is the mechanism which allows providers the right to appeal actions of ambetter such. Web use this form as part of the ambetter from coordinated care claim dispute/appeal process to dispute the decision made during the request for reconsideration process. Web all ambetter from arizona complete health members are entitled to a complaint/grievance and appeals process if a member is displeased with any aspect of services rendered.
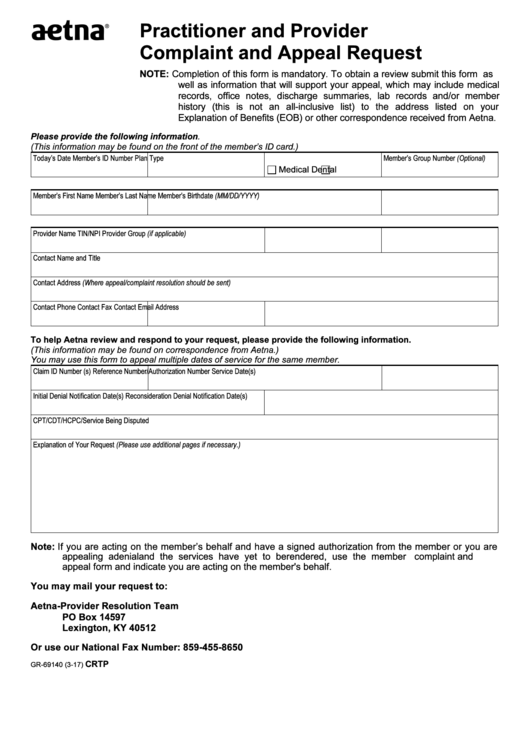
Fillable Form Gr69140 Aetna Practitioner And Provider Complaint And
You must file an appeal within 180 days of the date on the denial letter. Web as an ambetter network provider, you can rely on the services and support you need to deliver the highest quality of patient care. Web appeal you file an appeal in response to a denial received from ambetter from health net. Web ambetter provides the.
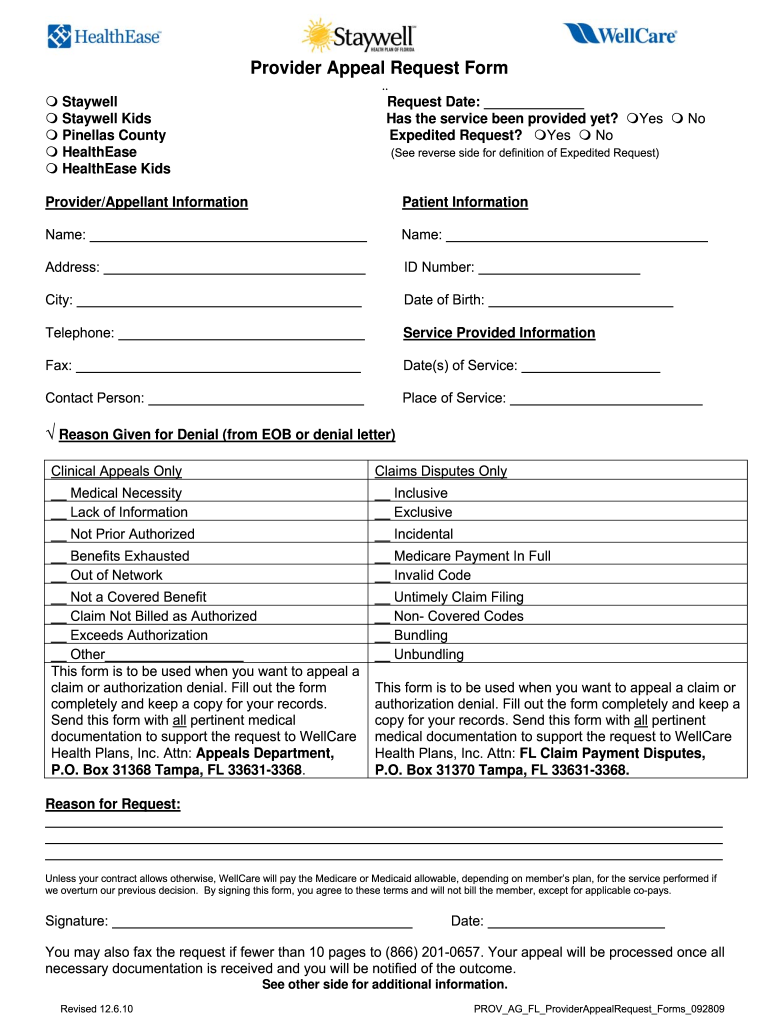
Wellcare Appeal Form Fill Online, Printable, Fillable, Blank pdfFiller
You must file an appeal within 180 days of the date on the denial letter. Web to ensure that ambetter member's rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. The requesting physician must complete an authorization request using one of the following methods: Web all ambetter from arizona complete health members are entitled to.
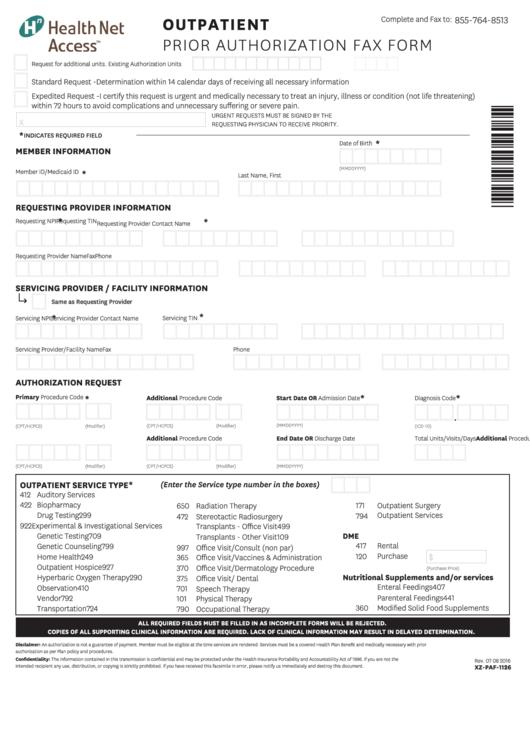
Outpatient Prior Authorization Fax Form printable pdf download
Web as an ambetter network provider, you can rely on the services and support you need to deliver the highest quality of patient care. Web provider complaint/grievance and appeal process. Web use this form as part of the ambetter from superior healthplanrequest for reconsideration and claim dispute process. Learn more about our health insurance. Web to ensure that ambetter member's.
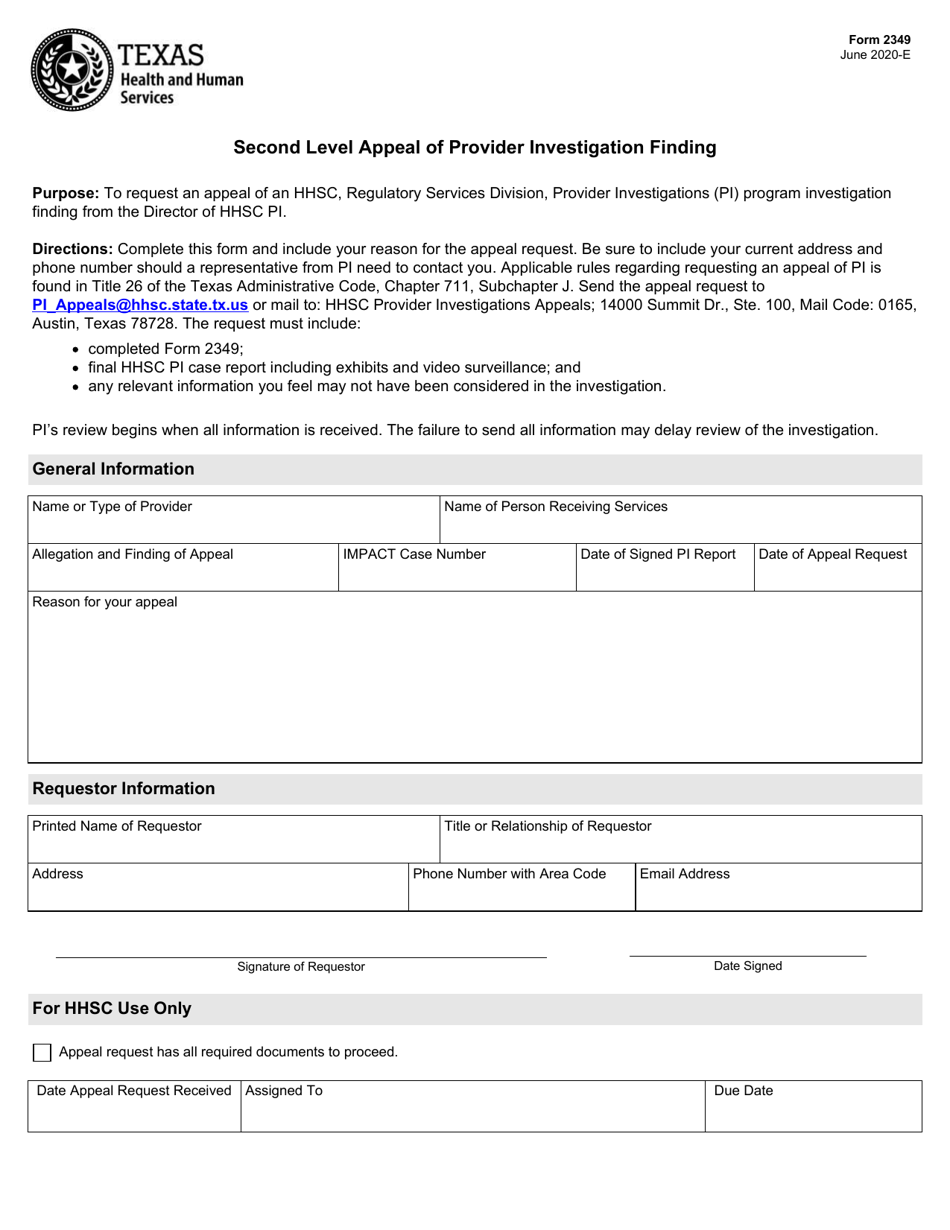
Form 2349 Download Fillable PDF or Fill Online Second Level Appeal of
Web prior to submitting a claim dispute, the provider must first submit a “request for reconsideration”. Web appeal you file an appeal in response to a denial received from ambetter from health net. See coverage in your area; Claim reconsideration claim appeal authorization appeal provider name. Web all ambetter from arizona complete health members are entitled to a complaint/grievance and.
Ambetter Agent Resources Plans And Client Brochures
Web provider reconsideration and appeal request form use this form to request one of the following: Learn more about our health insurance. Web use this form as part of the ambetter from coordinated care claim dispute/appeal process to dispute the decision made during the request for reconsideration process. Web ambetter provides the tools and support you need to deliver the.
Free Arkansas Medicaid Prior (Rx) Authorization Form PDF eForms
The completed form can be returned by mail or fax. Web use this form as part of the ambetter from coordinated care claim dispute/appeal process to dispute the decision made during the request for reconsideration process. All fields are required information. Web ambetter provides the tools and support you need to deliver the best quality of care. The claim dispute.
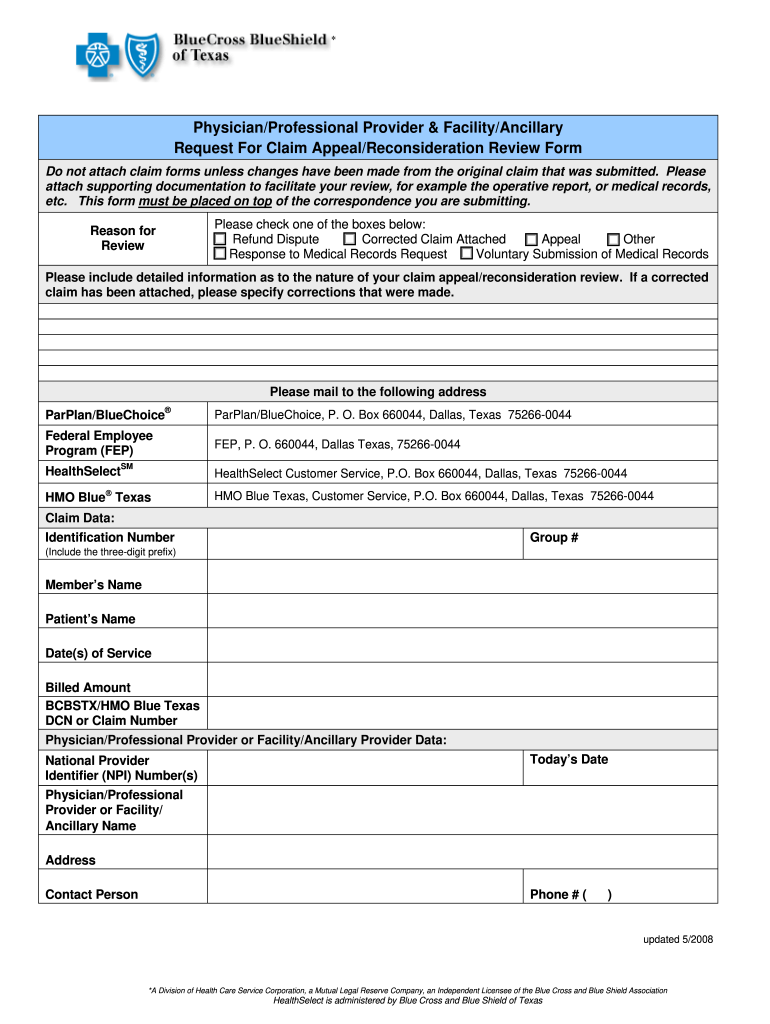
Texas Bcbs Provider Appeal Fill Out and Sign Printable PDF Template
Claim reconsideration claim appeal authorization appeal provider name. Web provider reconsideration and appeal request form use this form to request one of the following: All fields are required information. Web provider request for reconsideration and claim dispute form use this form as part of the ambetter from sunshine health request for reconsideration and. Reference materials 2023 provider & billing manual.
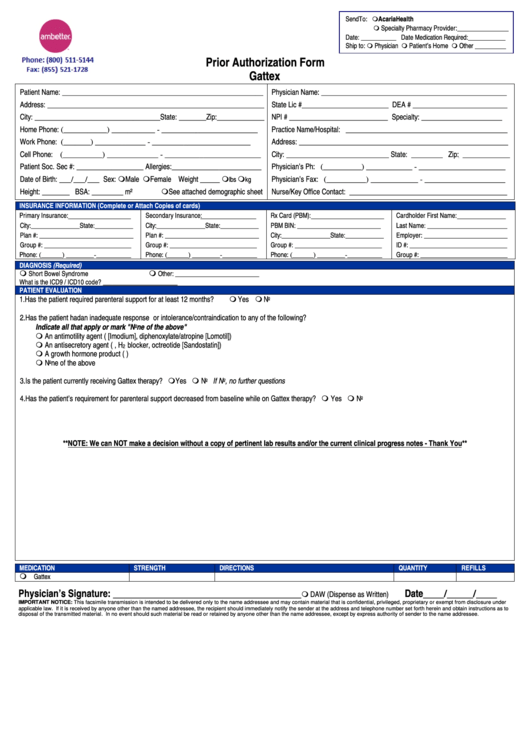
Ambetter Prior Authorization Form Gattex printable pdf download
Web outpatient prior authorization fax form (pdf) outpatient treatment request form (pdf) provider fax back form (pdf) applied behavioral analysis authorization form (pdf). Web use this form as part of the ambetter from superior healthplanrequest for reconsideration and claim dispute process. This could be a denial of coverage for requested medical care or for a claim you filed for. Web.
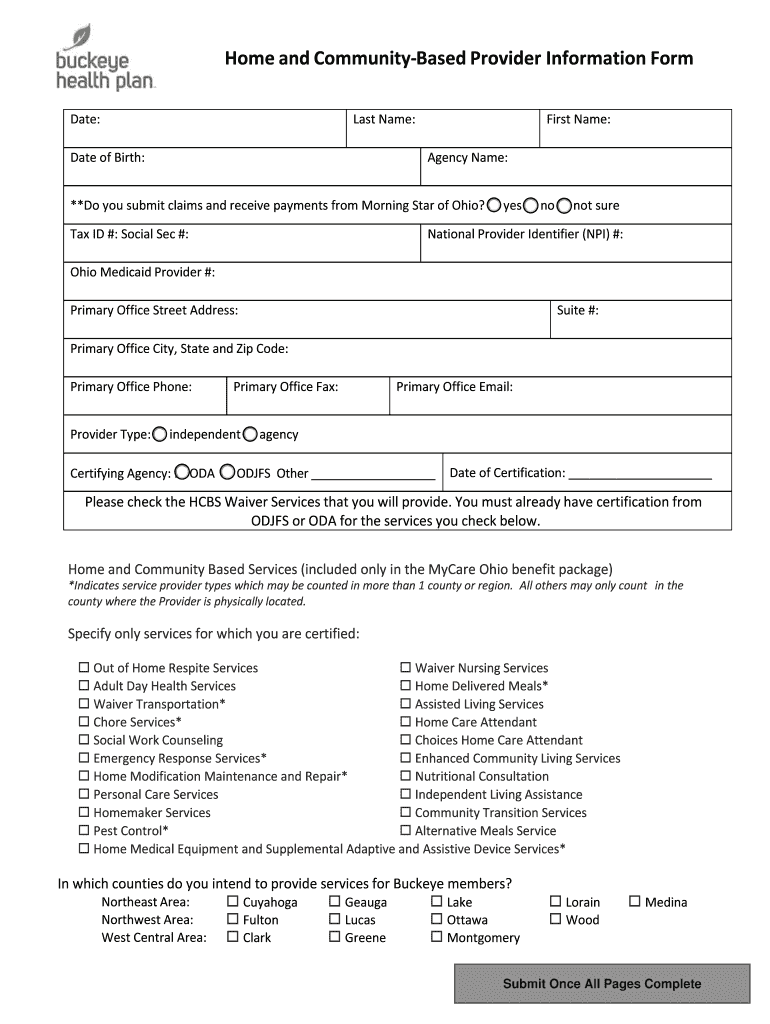
Buckeye Waiver Fill Out and Sign Printable PDF Template signNow
Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy: Web use this form as part of the ambetter from coordinated care claim dispute/appeal process to dispute the decision made during the request for reconsideration process. Web ambetter provider reconsiderations, disputes and complaints (cc.um.05.01) to see if the case qualifies for medical necessity review. An appeal is the mechanism.
Envolve Vision Newsletter Volume 6 Issue 3 National English
Web use this form as part of the ambetter from coordinated care claim dispute/appeal process to dispute the decision made during the request for reconsideration process. See coverage in your area; The completed form can be returned by mail or fax. Log in to the nch provider web portal at. All fields are required information.
Web Provider Reconsideration And Appeal Request Form Use This Form To Request One Of The Following:
Web provider complaint/grievance and appeal process. Reference materials 2023 provider & billing manual (pdf) 2022 provider & billing. See coverage in your area; Log in to the nch provider web portal at.
All Fields Are Required Information.
Web to ensure that ambetter member's rights are protected, all ambetter members are entitled to a complaint/grievance and appeals process. Disputes of denials for code editing policy. The claim dispute must be submitted within. Learn more about our health insurance.
An Appeal Is The Mechanism Which Allows Providers The Right To Appeal Actions Of Ambetter Such.
This could be a denial of coverage for requested medical care or for a claim you filed for. Web as an ambetter network provider, you can rely on the services and support you need to deliver the highest quality of patient care. Web use this form as part of the ambetter from coordinated care claim dispute/appeal process to dispute the decision made during the request for reconsideration process. Web provider request for reconsideration and claim dispute form use this form as part of the ambetter from sunshine health request for reconsideration and.
Web Use This Form As Part Of The Ambetter From Superior Healthplanrequest For Reconsideration And Claim Dispute Process.
Use your zip code to find your personal plan. The requesting physician must complete an authorization request using one of the following methods: Web outpatient prior authorization fax form (pdf) outpatient treatment request form (pdf) provider fax back form (pdf) applied behavioral analysis authorization form (pdf). Web prior to submitting a claim dispute, the provider must first submit a “request for reconsideration”.