Aetna Medicare Appeal Form For Providers
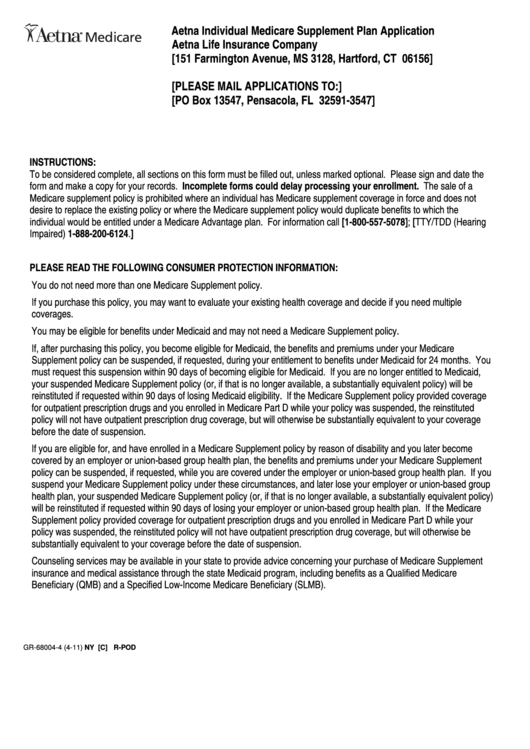
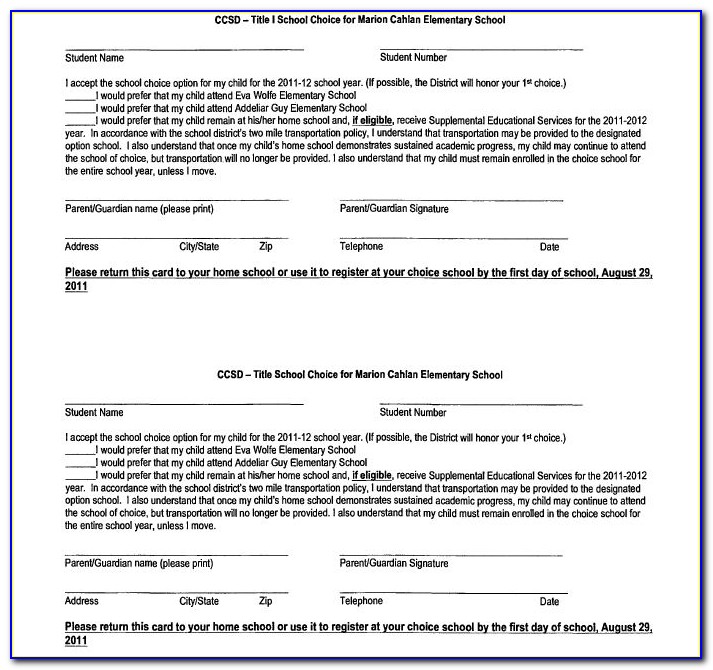
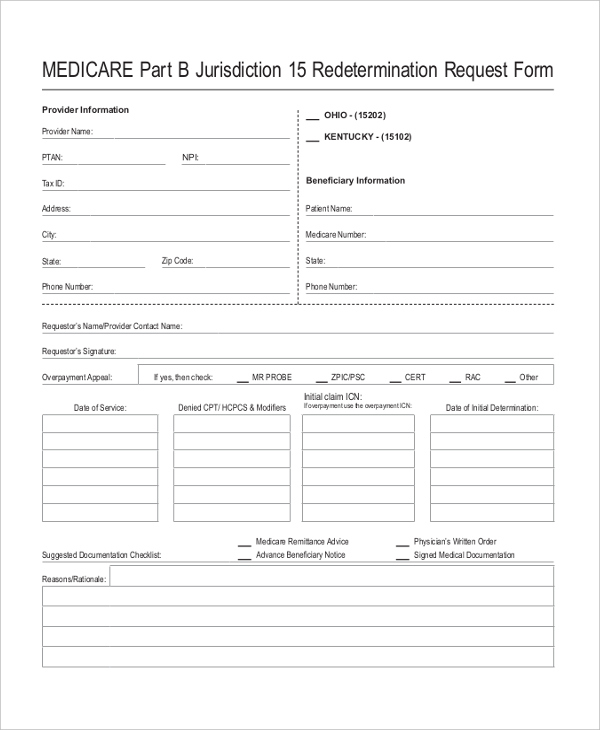
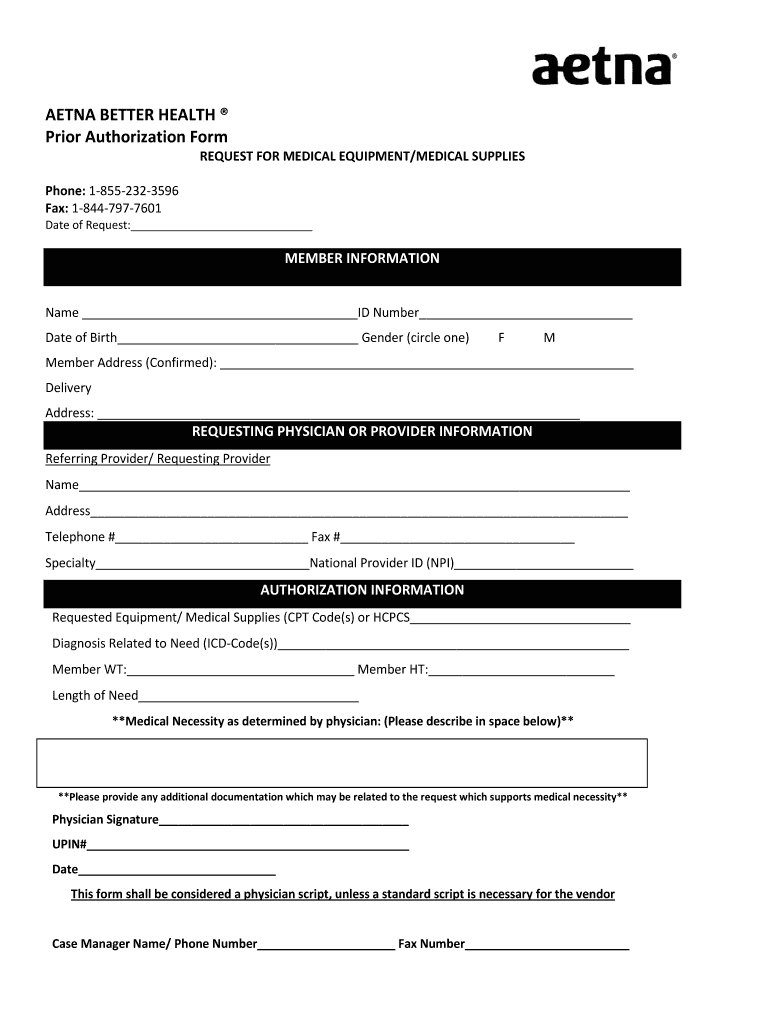
Aetna Medicare Appeal Form For Providers - Payment appeals for contracted provider requests. Web provider appeals dispute & appeal process: % change approved status effective date aetna life. Because aetna medicare (or one of our delegates) denied your request for. Web providers in the aetna network have the right to appeal denied medical item or service authorizations or medicare part b prescription drug for members. Make sure to include any information. Web as an aetna medicare member, you have the right to: To obtain a review, you’ll need to submit this form. Your doctor may ask us for an appeal on your behalf. Callers outside california and those in california (area codes 213 or 310), may contact the consumer.
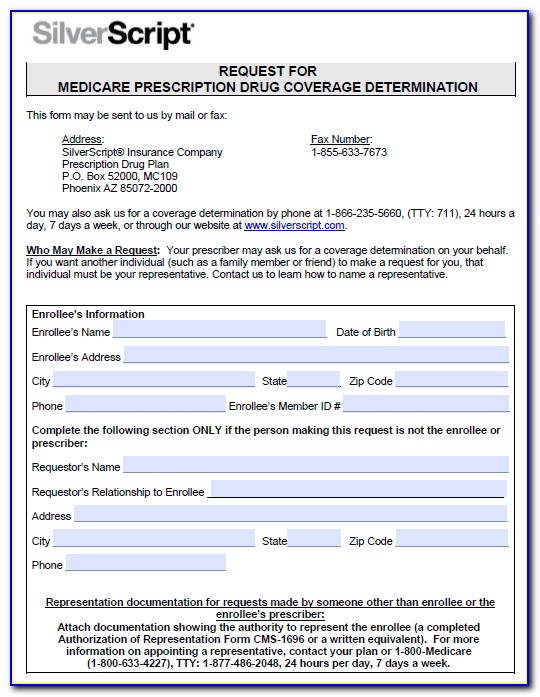
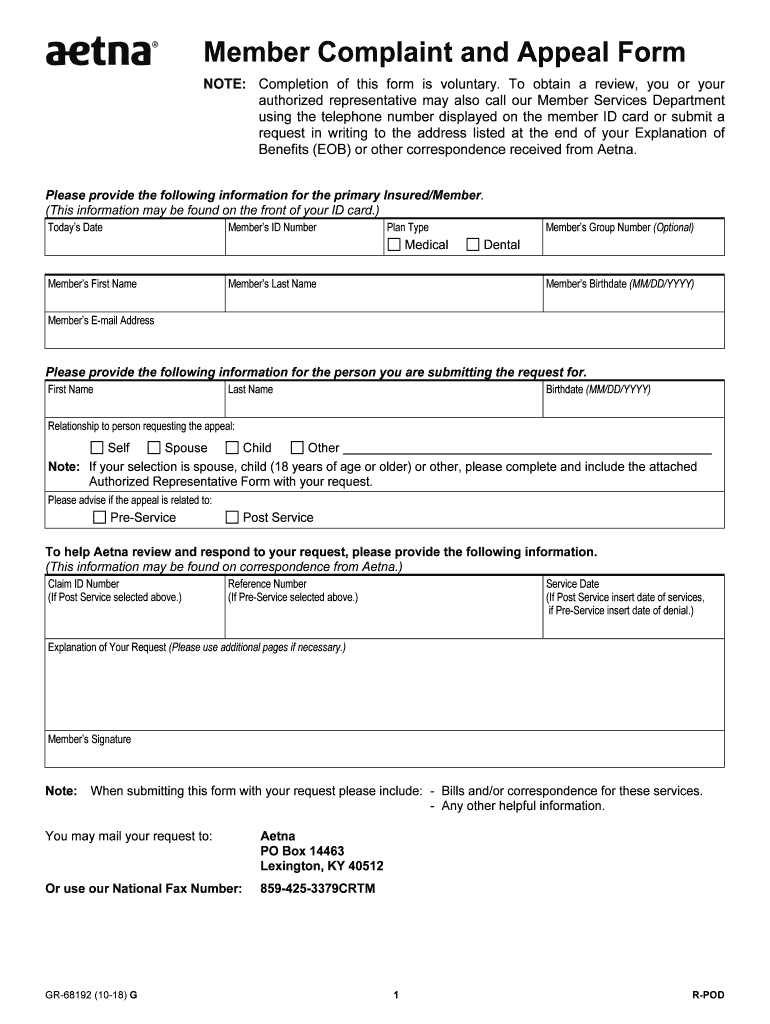
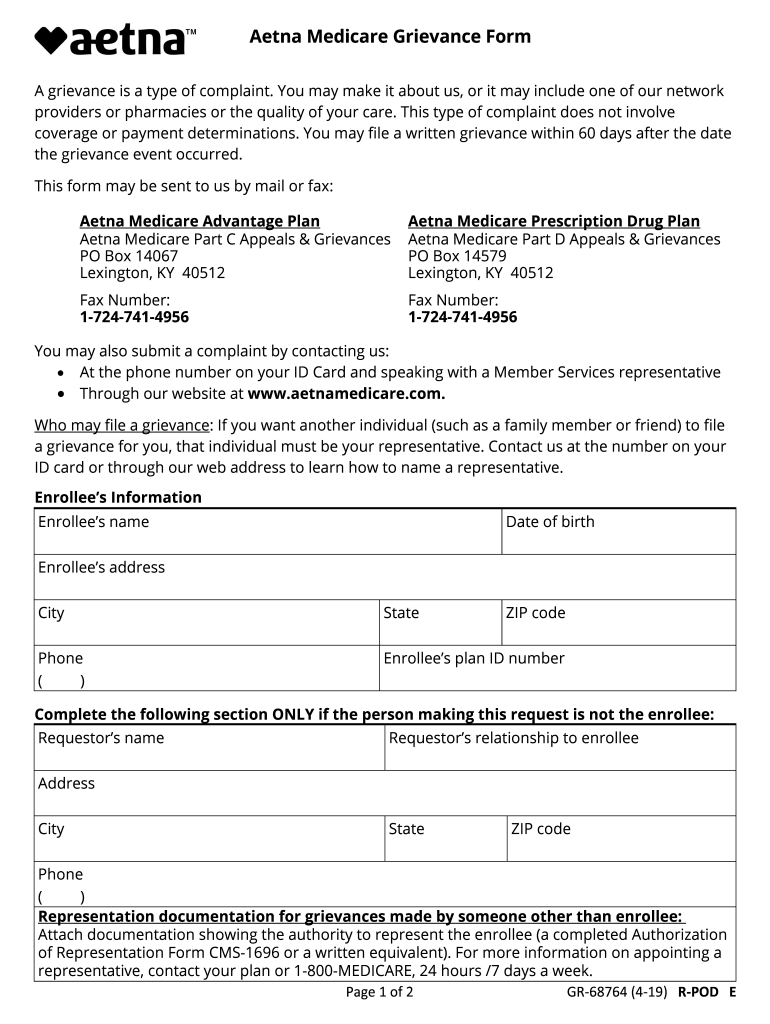
Web request for an appeal of an aetna medicare advantage (part c) plan claim denial. Who may make a request: Web complaint and appeal form. Web requesting an appeal (redetermination) if you disagree with medicare’s coverage or payment decision. You must complete this form. Appeals must be submitted by mail/fax, using the provider complaint and appeal form. In some cases, we may allow exceptions for a. Payment appeals for contracted provider requests. Web provider appeals dispute & appeal process: Or use our national fax number:
Web complaint and appeal form. Who may make a request: Web requesting an appeal (redetermination) if you disagree with medicare’s coverage or payment decision. Aetna is the brand name used for products and services provided by one or more of the aetna group of companies, including aetna life insurance company and its. Because aetna medicare (or one of our delegates) denied your request for. If you have a dispute around the rate used for payment. Web 2024 aetna life ins. These changes do not affect member appeals. Callers outside california and those in california (area codes 213 or 310), may contact the consumer. To obtain a review, you’ll need to submit this form.
Fill Free fillable Aetna Health Insurance PDF forms
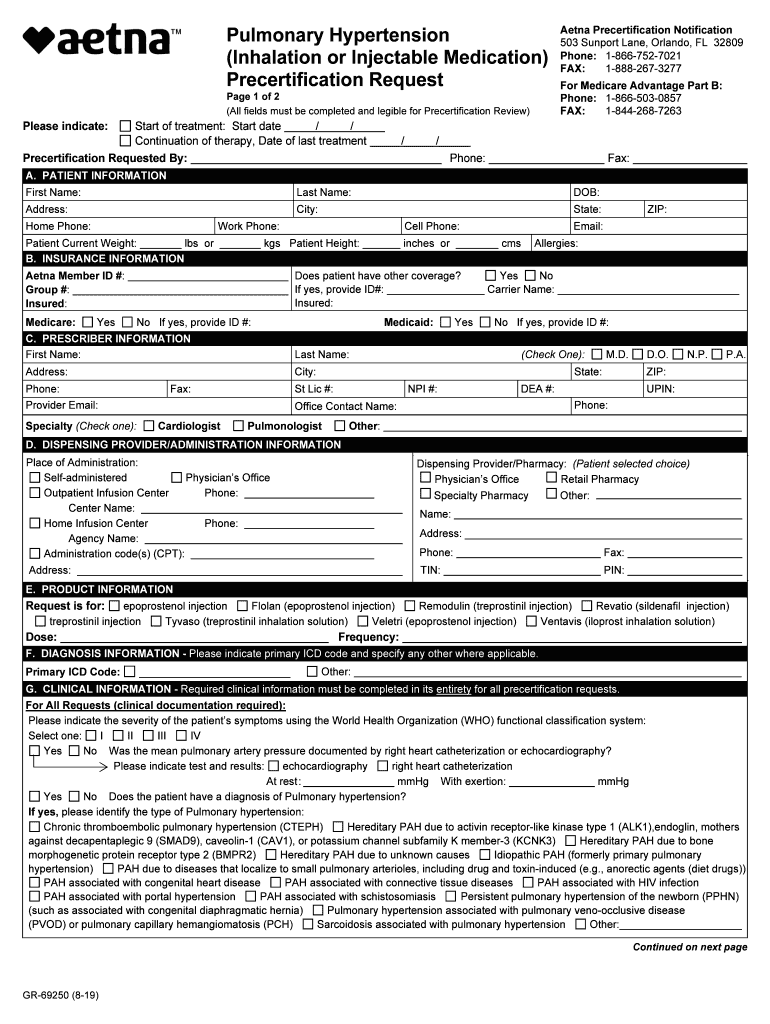
Because the society ditches office work, the completion of paperwork more and. Web providers in the aetna network have the right to appeal denied medical item or service authorizations or medicare part b prescription drug for members. Ask for coverage of a medical service or prescription drug. Aetna medicare part c appeals & grievances po box 14067 lexington, ky 40512..
Aetna Medicare Medication Prior Authorization Form Form Resume
You may mail your request to: Web providers in the aetna network have the right to appeal denied medical item or service authorizations or medicare part b prescription drug for members. Web complaint and appeal form. Aetna medicare part c appeals & grievances po box 14067 lexington, ky 40512. To obtain a review, you’ll need to submit this form.
Member aetna com membersecure assets pdfs forms 68192 pdf Fill out
(this information may be found on the front of the member’s id card.) today’s date member’s id number plan type member’s group. % change approved status effective date aetna life. This form may be sent to us by mail or fax: Aetna is the brand name used for products and services provided by one or more of the aetna group.
Aetna GR69250 2019 Fill and Sign Printable Template Online US
Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial. To obtain a review, you’ll need to submit this form. Web 4.8 satisfied 375 votes what makes the aetna provider complaint and appeal form legally binding? Web you can call us at: % change approved status effective date aetna life.
Prior Authorization Form For Medicare Advantage Universal Network
Who may make a request: Web please provide the following information. To obtain a review, you’ll need to submit this form. Exceptions apply to members covered under. Make sure to include any information.
Aetna Medicare Complaint Team Fill Out and Sign Printable PDF
Web complaint and appeal form. Payment appeals for contracted provider requests. Web as an aetna medicare member, you have the right to: Web complaint and appeal request note: Aetna medicare part c appeals & grievances po box 14067 lexington, ky 40512.
Aetna Life Insurance Medicare Supplement Aetna LeClair Group
Web complaint and appeal request note: Callers outside california and those in california (area codes 213 or 310), may contact the consumer. Payment appeals for contracted provider requests. Web your denial to ask us for an appeal. Who may make a request:
Medicare Medical Claim Reimbursement Form Aetna Form Resume
This form may be sent to us by mail or fax: These changes do not affect member appeals. Or use our national fax number: Web as an aetna medicare member, you have the right to: Web complaint and appeal request note:
FREE 10+ Sample Medicare Forms in PDF MS Word
Web you can call us at: Because aetna medicare (or one of our delegates) denied your request for. You may mail your request to: Aetna medicare part c appeals & grievances po box 14067 lexington, ky 40512. Web consumers may call or write the bureau to have claims reviewed.
Aetna better health prior authorization form Fill out & sign online
You must complete this form. Your doctor may ask us for an appeal on your behalf. As an aetna dentist, you'll be part of a strong national network with access to millions of members. Web your denial to ask us for an appeal. Because the society ditches office work, the completion of paperwork more and.
To Obtain A Review, You’ll Need To Submit This Form.
These changes do not affect member appeals. Make sure to include any information. Because aetna medicare (or one of our delegates) denied your request for. You may mail your request to:
Web Working With You To Help Your Patients.
As an aetna dentist, you'll be part of a strong national network with access to millions of members. Web 4.8 satisfied 375 votes what makes the aetna provider complaint and appeal form legally binding? Web complaint and appeal request note: Web all appeals must be submitted in writing, using the aetna provider complaint and appeal form.
Because Aetna Medicare (Or One Of Our Delegates) Denied Your Request For Payment Of.
Web as an aetna medicare member, you have the right to: Callers outside california and those in california (area codes 213 or 310), may contact the consumer. % change approved status effective date aetna life. In some cases, we may allow exceptions for a.
Because The Society Ditches Office Work, The Completion Of Paperwork More And.
You'll benefit from convenient tools,. Web request for an appeal of an aetna medicare advantage (part c) plan authorization denial. Who may make a request: Web your denial to ask us for an appeal.